Dr Quang Dao
Discoid meniscus is a congenital variant of the meniscus which can affect its size, shape and stability. Most often, it affects the lateral meniscus.
Incidence
It is a frequent finding in the Asian population with an incidence of up to 20%. In Caucasians, the incidence is 3-5%. It is slightly more common in females.
Pathoanatomy
A discoid meniscus is thicker and have a poorer blood supply than the normal meniscus. It is also larger and covers more of the underlying tibial plateausurface. This exposes it to more load between the femoral condyle and tibial plateau. Electron microscopy have demonstrated that a discoid meniscus hasdecreased number of collagen fibres and which are also disorganised. These factors make a discoid meniscus more fragile, easier to tear and less likely to heal following repairs.
Classification
There are 3 types of discoid menisci according to the Watanabe classificationwhich is based on arthroscopic findings.
Type I – complete and stable. The meniscus is very thick and appears like a block of tissue. It covers the entire tibial plateau. It is stable to probing during surgery.
Type II – partial and stable. The meniscus covers up to 80% of the tibial plateau. It is not as thick as type I. It is also stable to probing.
Type III – unstable Wrisberg variant. It is unstable when probed. This instability is due to the lack of the normal meniscotibial ligaments. These are fibres which normally attach the meniscus to the rim of the tibial plateau and thus provides stability. These type III menisci have the Wrisberg ligament present. This is a band of tissue connecting the back part of the meniscus to the medial femoral condyle.
Presentation
The classic presentation of a discoid meniscus is bulging of the joint line in flexion, clunking or popping of the knee in extension (snapping knee syndrome) and an inability to fully extend the knee. Pain, swelling and mechanical symptoms such as painful clicking, locking and giving way can occur when there is a tear. Discoid menisci can tear with minimal trauma, unlike its normal counterpart which often tears with sporting injuries.
Investigation
Radiographs are often normal. Sometimes with the type I complete discoid meniscus, x-rays may demonstrate a widened joint space, squaring of the femoral condyle, cupping of the tibial plateau and hypoplastic lateral tibial spine.
MRI is the preferred investigation tool for discoid menisci. On the coronal images, the meniscus is wider than 15mm or greater than 20% of the entire tibial plateau. On three consecutive 5mm thick sagittal images, there is continuity between the anterior and posterior horns (bowtie sign).
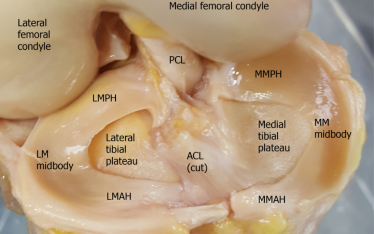
Arthroscopic Findings
Treatment
Conservative management with observation is indicated for asymptomatic discoid menisci. This approach is still appropriate even for those knees which are clunking but has minimal pain and absence of locking or giving way. It is advisable that these patients avoid high impact activities to reduce the risk of meniscal tears.
Symptomatic knees can be treated surgically by saucerisation, repair and stabilisation.
Saucerisation is reshaping of the discoid meniscus. Usually the excess central portion is excised, leaving a peripheral rim of 6-8mm. Often the torn part is located in the central portion and it gets removed in the process of saucerisation. If there is still a tear in the remaining peripheral portion, it can be repaired. In the unstable discoid meniscus, this remaining peripheral portion is sutured to the capsule.
It has been reported that meniscal resection in adolescents causes three times the rate of radiographic changes consistent with osteoarthritis after 30 years. Therefore, complete resection of the meniscus is avoided if possible.