Dr Quang Dao
Information for orthopaedic surgeons
Some patients still report rotatory instability following well performed anterior cruciate ligament reconstructions. This may be due to neglected concomitant injuries to the anterolateral structures of the knee.
In the last two decades there have been much research to provide anatomical and biomechanical data about these anterolateral structures. Surgical techniques have been developed to provide additional knee rotational stability.
The two main parts of the anterolateral aspect of the knee which provide rotational stability are the anterolateral ligament (ALL) and the iliotibial tract (ITT).
Anterolateral Ligament
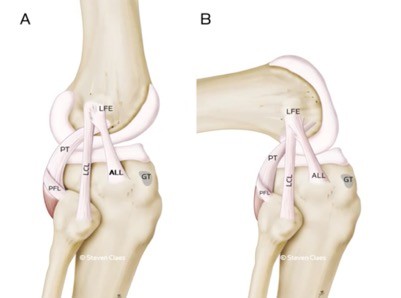
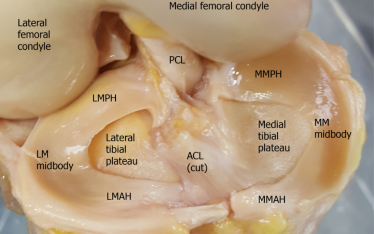
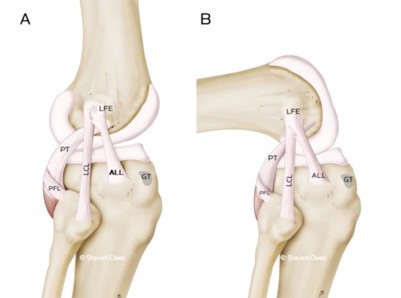
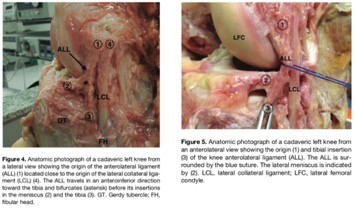
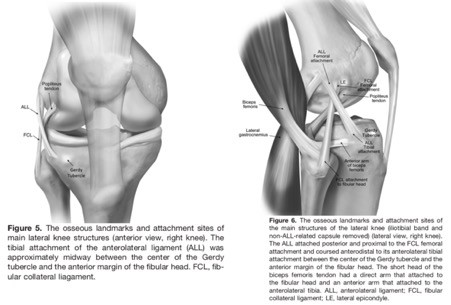
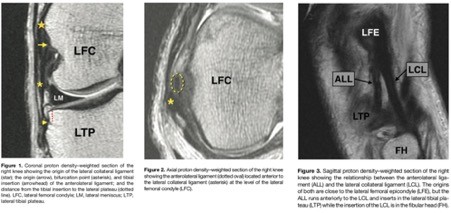
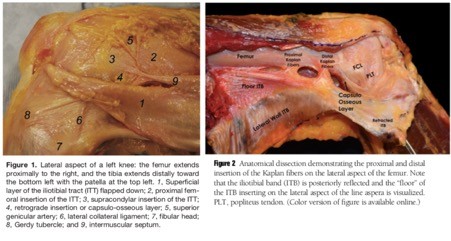
Steven Claes (J Anat 2013) identified the ALL in 40 of 41 cadaveric knees. He pointed out that from its origin at the lateral femoral epicondyle (LFE), the anterolateral ligament (ALL) runs superficial to the lateral collateral ligament (LCL). It then bifurcates, with one attachment to the lateral meniscus and the other into the proximal tibia about halfway between Gerdy’s tubercle and the fibular head.
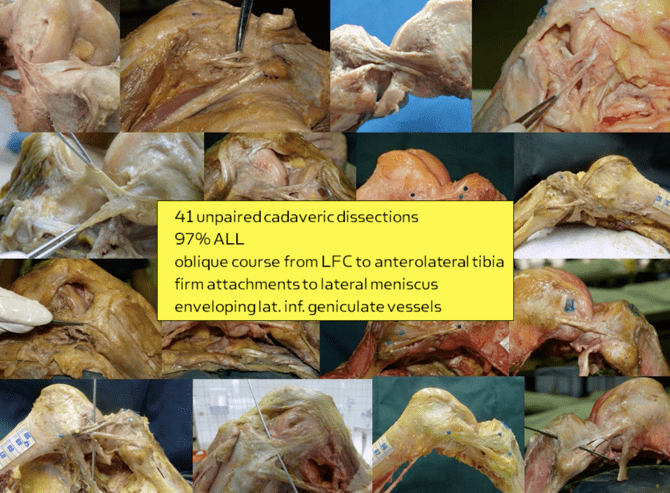
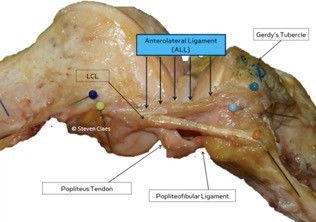
The lateral inferior genicular artery (LIGA) runs between the lateral meniscus and the ALL.
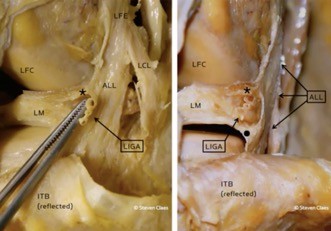
Helito et al (OJSM 2015) identified to femoral origin of the ALL is at the centre of the lateral femoral epicondyle and slightly anterior and distal to the FCL attachment point. It bifurcates and attach to the lateral meniscus and lateral tibial plateau.
In his dissection study, Sonnery-Cottet showed that the ALL is a thin structure and it fans out to its tibial insetion.

The tibial attachment of the ALL is consistent reported as between Gerdy’s tubercle and the fibular head. However, different authors have reported slight variations in its femoral origin. It is usually described as either anterior and distal to the femoral attachment point of the fibular collateral ligament (FCL) (Claes,Vincent, Caterine, Helito) or slightly proximal and posterior to it (Kennedy, Caterine, Spencer, Dodds, Kittl).
Spencer et al (AJSM 2015) showed in their dissection study that the ALL is superficial to the FCL. It originates from just proximal and posterior to the FCL origin. They found that the ALL assists the ACL in anterolateral rotation.
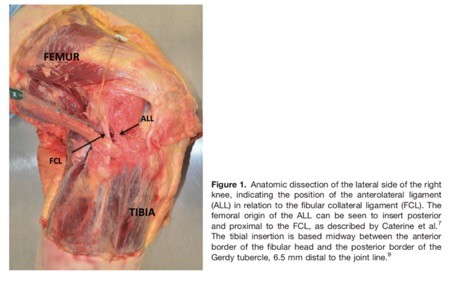
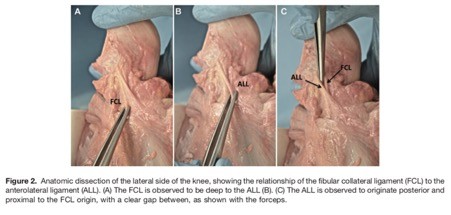
Kennedy et al (AJSM 2015) examined 15 nonpaired cadaveric knees. The ALL was identified in all the specimens. Its point of origin is proximal and posterior to the FCL femoral attachment. Its tibial attachment was between the centre of Gerdy’s tubercle and the anterior margin of the fibular head.
Anterolateral Ligament Foetal Cadaveric Dissection
There is evidence that the ALL is present in foetal cadaver dissection and histologic examination.
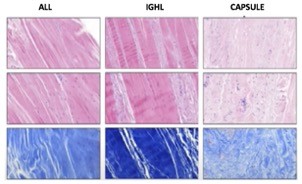
Anterolateral Ligament Histology
Claes et al have shown that the ALL is biomechanically and histologically different to the anterolateral joint capsule of the knee. He believes that it is not just a thickening of the capsule but rather a distinct ligament similar to the inferior glenohumeral ligament (IGHL) of the shoulder.
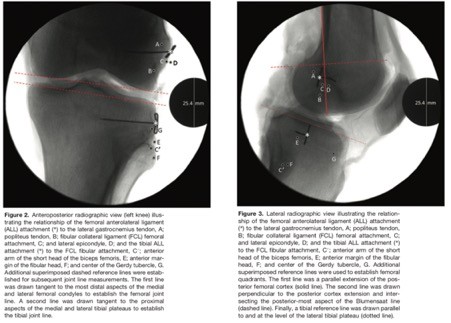
Anterolateral Ligament X-rays and MRI
Kennedy et al (AJSM 2015) provided radiographic landmarks of the ALL as well as attachment points of the other lateral structures.
The ALL can be seen on MRI scans. However, for best visualisation, the slice thickness should be less than 1.5mm with no spaces in between. Proton density (PD) is the best sequence.

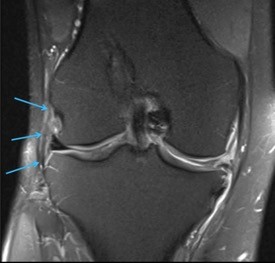
Claes found almost 80% of ACL injured knees have MRI findings of an injured ALL. Most of these occur at the tibial insertion or mid-substance.
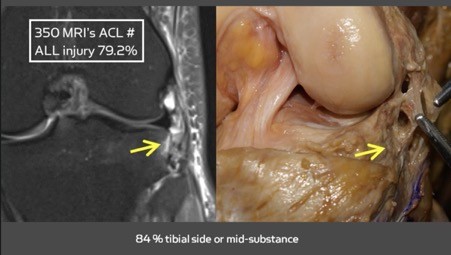
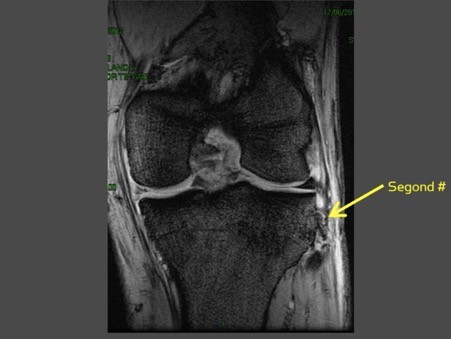
Helito et al (KSSTA 2017) found ALL injuries in 39.5% of MRI scans in knees with ACL ruptures. Only 6% had a Segond fracture. This indicates that only a small proportion of ALL injuries will have a bony avulsion.
Anterolateral Ligament Biomechanics
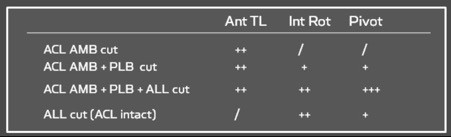
Claes showed that additional cutting of the ALL after the ACL has been transected, increases the amount of tibial internal rotation. It also produces a high grade pivot shift test. Isolated sectioning of the ALL also increases the tibial internal rotation but produces a less explosive pivot shift.
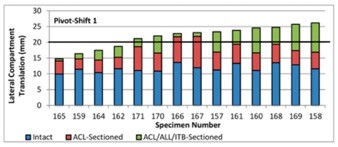
Noyes et al (JBJS 2017) used a robotic simulator on 14 cadaveric knees. Their sequential sectioning study showed that the ALL and Iliotibial band (ITB) are secondary restraints to tibial internal rotation. Cutting these 2 structures increase the amount of internal rotation after the ACL has been sectioned. In 8 of their 14 specimens, cutting of these 2 structures in addition to the ACL increases the lateral compartment translation to beyond 20mm, which is a value necessary for a grade 3+ pivot shift. Also note that a grade 3+ pivot shift test is absent in 4 cases even after cutting of all 3 structures.
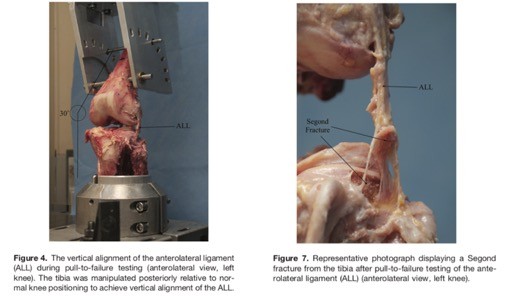
Kennedy et al (AJSM 2015) recorded the mean maximum load to failure of the ALL was 175N. Six of the cases demonstrated avulsing the tibial attachment, representing a Segond fracture.
Iliotibial Tract
Kittl et al (AJSM 2015) reported that the deep fibres of the iliotibial tract (ITT) provided the most restraint to internal tibial rotation at low knee flexion angles. The superficial fibres provided more restraints to internal rotation at higher flexion angles. Overall the entire ITT is most important at 0-90 degrees flexion. In their dissection and robotic simulation study, the anterolateral ligament only had a minor role in restraining tibial internal rotation.
Lording et al (KSSTA 2017) have shown in their cadaveric dissection study that cutting the superficial and deep parts of the iliotibial tract increases tibial anterior translation, adduction and internal rotation.
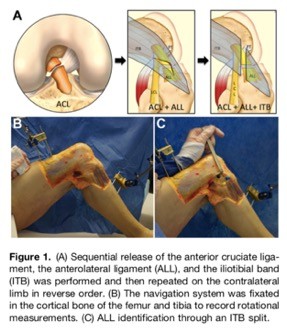
Sonnery-Cottet et al (AJSM 2016) performed sequential sectioning of the ACL, ALL and ITB in one knee and then in the reverse order in the contralateral knee. Sectioning of the ALL after sectioning the ACL or ITB, increases tibial internal rotation.