The anterior cruciate ligament (ACL) is one of the major ligaments of the knee. It sits deep inside the knee. It is made of collagen fibres and acts like a rope connecting the tibia (shin bone) to the femur (thigh bone). It guides the knee in its normal motion. More importantly it stabilises the knee. The ACL has 2 separate bundles – anteromedial (AM) and posterolaterl (PL).
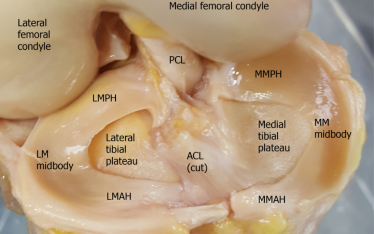
MFC – medial femoral condyle
LFC – lateral femoral condyle
AM – anteromedial bundle of the ACL
PL – posterolateral bundle of the ACL
The ACL is covered by a vascularised layer of synovium
How is the ACL injured?
The ACL is usually ruptured during sporting, work or motor vehicle accidents. The most common sports causing ACL tears are soccer, football, netball and skiing. It is usually due to non-contact mechanisms where the foot is planted in the ground and the rest of the body continue to move or twist causing an abnormal force through the knee. Sometimes the injury is by direct contact such as in a football tackle.
Double click on the image to PLAY video showing injuries causing ACL tears
How Do Patients Present?
At the moment of injury, patients often hear or feel a popping sound in the knee. The knee usually collapses and the patient falls to the ground. There is significant immediate pain. The patient struggles to get up and walk. The knee would give way immediately in those that try to resume their sporting activity. There is often swelling in the knee over the next 24 hours.
Why is There Pain?
The ruptured ACL itself causes minimal pain. Pain is due to injuries of the surrounding tissues such as meniscal tears, fractures to bone and cartilage, ruptures of other ligaments, bleeding and inflammation.
Why is There Swelling?
Swelling usually occurs within 24 hours of the injury. It is due to disruption of the blood vessels which run along the ACL. It can also be the result of bleeding from a fracture of the thighbone or shinbone or tears of the capsule. If an aspiration were to be performed acutely to suck out the fluid, it would yield blood. Swelling which occurs later is a result of inflammation within the joint. Its appearance is more straw colour and can be blood stained.
What to Expect in the First Few Days?
With the significant pain and swelling, patients find it difficult to walk on the injured leg. They cannot fully straighten or bend the knee. The knee feels unstable when walking, especially while climbing the stairs.
What to Expect in the Next Few Weeks?
In isolated ACL injuries, pain and swelling will slowly improve and settle after 3-4 weeks. The knee has more movement and the patient experiences less instability when weight bearing during normal walking. Persistence of symptoms suggests other pathologies.
Patients may experience giving way or instability when they return to sports. Again, these episodes can cause pain and swelling.
How Should the Knee be Managed Initially?
Patients should be assessed by a doctor or experienced physiotherapist following any major knee injury. The doctor will thoroughly take your medical history and perform clinical examination. Radiographs will exclude any obvious fracture. The knee will then be managed according to the RICE principles – Rest, Ice, Compression and Elevation. A compression bandage will be applied and the knee will be placed in a brace. Frequent ice packing will help control pain and swelling. Patients are advised to use crutches and to elevate the injured knee as much as possible. Painkillers and anti-inflammatory medications will be prescribed. Based on the history, examination and x-ray results, MRI scans will be organised. An orthopaedic referral is usually required.
Once the diagnosis of an isolated ACL injury is confirmed, the brace is removed and early motion is encouraged. In multi-ligament injuries or if fractures are present, brace wearing may be prolonged.
How is the Ruptured ACL diagnosed?
The diagnosis is based on the symptoms and signs. The clinical examination may reveal a joint effusion, muscle wasting, positive Lachmann’s, anterior drawer and pivot shift tests. These are special tests to assess the integrity of the ACL. There may be localised tenderness due to other structural injuries such as meniscal tears or cartilage damage. Patients may also experience reduced motion.
Double click on image to PLAY video showing Lachmann, anterior drawer and pivot shift tests
X-rays may, on the rare occasion, demonstrate a small avulsion flake of bone from the outer and upper part of the tibia (shin bone). This lesion is called a Segond fracture. It is highly suggestive of a ruptured ACL. It is caused when there is excessive rotation of the tibia, stretching the joint capsule and pulling away a small flake of bone.
MRI scans are used to confirm the diagnosis. These scans can also detect other injuries.
MRI scans showing an intact ACL
MRI scans showing a ruptured ACL
Should All Patients Have Knee Reconstruction?
Not all patients will require surgery. ACL reconstruction is indicated if patients experience giving way with simple daily activities. It should also be considered in those planning on returning to cutting, pivoting or contact sports. Another indication is in patients with other pathologies such as meniscal tears requiring repair or those with more that one ligament ruptures.
Therefore, patients with isolated ACL injury, whose knee is currently stable and are not planning on any future strenuous activity, do not require reconstructive surgery.
What Happens if the Ruptured ACL is Not Reconstructed?
Many, but not all knees with ruptured ACL will experience instability. Several factors determine this. Knees are more likely to give way if there is additional ligament, meniscal or cartilage damage. The type of activity will also dictate the likelihood of instability. Cutting or pivoting sports and labor intensive work increases the risk, as well as poor neuromuscular control and being non-compliant with a well-planned rehabilitation program.
Instability prohibits patients from participating in their usual activity. Each time the knee gives way, it can potentially cause more damage to other structures such as the meniscus or articulating cartilage.
How is the Surgery Performed?
The surgery can be performed open or arthroscopically (keyhole). Usually, the patient is given general anaesthetics.
The injured ligament is removed and replaced by a graft. This graft can come from the patient’s own tissue, such as the hamstrings, patellar tendon, quadriceps tendon or iliotibial band. It can also come from a live or deceased donor. It can also be a synthetic material. The choice of graft is dependent on your surgeon’s preference as well as what is available. Graft harvesting is performed open or through a small incision with the assistance of special instruments. The graft is prepared. Its length and width are measured.
Hamstring graft
Bone-patellar-bone graft
Synthetic graft
Arthroscopic examination of the knee is performed to assess the ACL tear and other structures such as the meniscus and cartilage. Surgery to address these other pathologies is performed before ACL bony tunnels are created. In most cases one femoral and one tibial bony tunnel is drilled. The size of the tunnels is appropriate to receive the graft that was prepared earlier. The graft is passed through these tunnels and secured with special devices such as a button, screw or staple. These devices are made of metal, inert plastics or bio-absorbable material.
Local anaesthetics are infiltrated into the wound, along the harvested tendon, around the femoral nerve or adductor canal to provide good pain relief immediately after surgery.
What is the Post-operative Care?
Some surgeons allow their patients to go home on the same day as the surgery. Others may elect to keep them overnight to provide closer observation and pain control.
Pain and swelling management are most important in the immediate post-operative period. Compression bandage, ice and elevation are essential in the first few days. In isolated ACL reconstructions, most surgeons allow their patients to commence early full weight bearing. In those cases where ACL reconstruction is combined with meniscal repair or cartilage surgery, some surgeons will keep their patients non-weight bearing for the initial period. This is usually 6 weeks.
Early range of motion exercises and muscle activation are encouraged during the initial period. Strengthening, balance training, and return to function are some other important aspects of the rehabilitation process. Physiotherapy plays a crucial role in this rehabilitation process.
When Can Patients Return to Sports?
The surgeon will determine when patients can return to sports. There are specific goals that must be met.
- Completed the rehabilitation program
- Pain free
- Full motion
- Stable knee
- Full strength when compared to other knee
- Adequate hamstrings to quadriceps strength ratio
- Agility T test
- Hop test
This usually takes 12 months to achieve.
What are the Risks and Complications of Surgery?
Some of the more common complications include
- Reactions to general and local anaesthetics
- Infection
- Injuries to nerves and blood vessels
- Bleeding
- Blood clots
- Pain
- Stiffness
- Graft failure
- Persistent instability
What I Do for You, as My Patient?
After a thorough history taking and clinical examination, I will arrange for MRI scans of your knee. Having your MRI scans organised by your family doctor before the consultation would definitely speed up the process. Please remember to bring the actual films of your scans (in addition to the report) for assessment.
If we decide that non-surgical treatment is best for you, then I will arrange for a formal referral to a local physiotherapist. I will review you over the next few months to ensure that you can safely return to your normal daily activities.
If we feel that surgery is required, then an in depth discussion about the surgery takes place.
I use your hamstrings as the source of graft. Most of the time we take your semitendinosis tendon. We quadruple the tendon using the Arthrex Graftlink technique. Tunnels are created arthroscopically in the femur and tibia. The graft is passed through the tunnels and into the knee joint. It is fixed at both cortical surfaces using Tightrope buttons.
Quadrupled semitendinosis tendon as graft
Graft secured with Tightropes & buttons
I keep my patients overnight for pain management, close observation and early physiotherapy.
I review you at 2 weeks, 6 weeks, 6 months, 12 months and sometimes 2 years.